Clean Claims
Claimcheck
An AI-powered claims assistant that helps practices submit stronger claims, faster, and with fewer headaches.
Join the Waitlist
Smarter Submissions, Faster Payments
Claimcheck™ automatically reviews, corrects, and strengthens claims, so more get approved and practices get paid faster.
Works for Practices, Not Insurers
Checkcheck™ embeds with your PMS and works ethically with clearinghouses to strengthen claims.




























































Supported Software
- PlanetDDS
- Eaglesoft
- Fuse
- Open Dental
- Curve Dental
- Patterson Dental
- Romexis
- Vatech
- Medit
- Dentally
- Exact
- Oryx
- Sota Cloud
- Ora
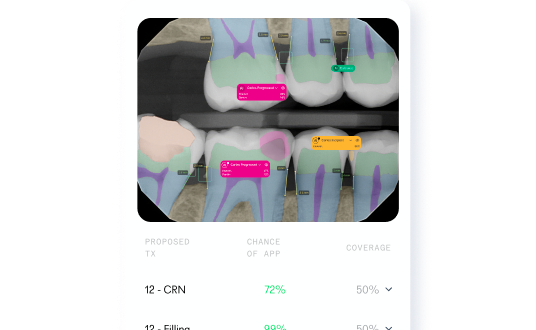
Automatically Attaches the Right Proof
Claimcheck selects and annotates the best radiolobic evidence to support approval.

Tailors Narratives for Every Payor
Auto-generates and verifies claim narratives to meet each payor's unique criteria.

Knows Every Payor’s Digits
Claimcheck’s exhaustive dataset cross-checks diagnostic codes with payor-specific criteria to get claims through faster.

FAQ
Is Claimcheck easy for staff to use?
Yes, intuitive web-based UI with guided submission, instant feedback, and visual error/warning flags for insurance criteria.
Does it work with my current software?
Claimcheck supports direct integration with leading PMS platforms and imaging systems, using APIs and standardized export formats.
How is data protected?
All patient and claim data is encrypted, HIPAA/GDPR compliant, and stored securely in regional data centers.
How does it improve documentation?
It ensures all codes are correct, clinical images are present, and required evidence is attached before claims are sent. Consistency is guaranteed for each insurer’s unique requirements.
Can Claimcheck help with denied claims/appeals?
Yes, it identifies missing documentation and helps prepare robust appeals, reducing administrative delays.