Everything you need to know to start using AI in your practice is here––from setting up Second Opinion for the first time to adjusting the AI settings to suit your needs.
My patient says “No insurance on file” but they do have insurance?
Please double check that the insurance information is correctly placed within your practice management software and the patient’s member ID is accurately filled out. This information will update in Precheck on the next re-sync (overnight). To learn more, find your practice management software below.
The Eligibility Member ID pulls from the Subscriber ID field under the Primary Insurance Plan in Open Dental.

To edit, double click the cell next to Subscriber ID, then add the updated member ID into the Subscriber ID field under Subscriber Information
Payer ID
The Eligibility Payer ID pulls from the Payer ID field in Open Dental.


Member ID
The Eligibility Member ID pulls from the Primary Member ID field within Preferences in Eaglesoft.
Click here to learn why we use the Primary Member ID in Eaglesoft versus the Carrier ID.

Payer ID
The Eligibility Payer ID pulls from the Claim Payer ID field in Eaglesoft.

Member ID
The Eligibility Member ID pulls from the Subscriber ID # field within Dentrix.

Payor ID
The Eligibility Payor ID pulls from the Payor ID column in Dentrix.

Because of our unique verification method checking directly with carriers and multiple clearinghouses, eligibility information may be available without a direct connection. Check to see if your patient has a summary available containing the information needed. If no information is available, the carrier is not supported and other avenues of verification will be needed.


Precheck continues to work on adding more payer options to its database. This current list is accurate as of 4/14/2025.
View list of supported payors ➜
At this time we only support 1 NPI per office.
From within your Pearl platform, go to Members in the settings.



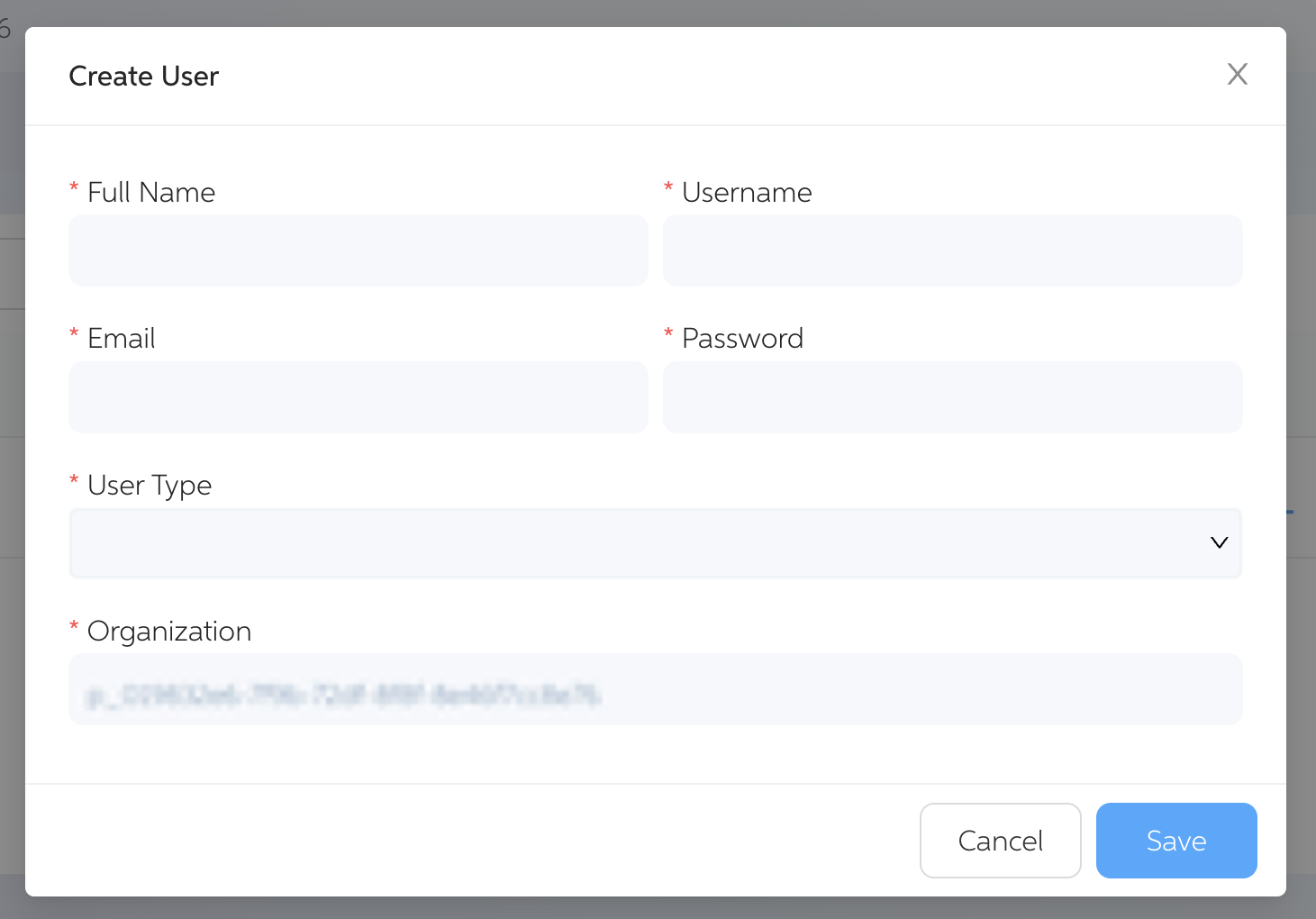
Complete all required fields to set up the new user account.
Choose one:

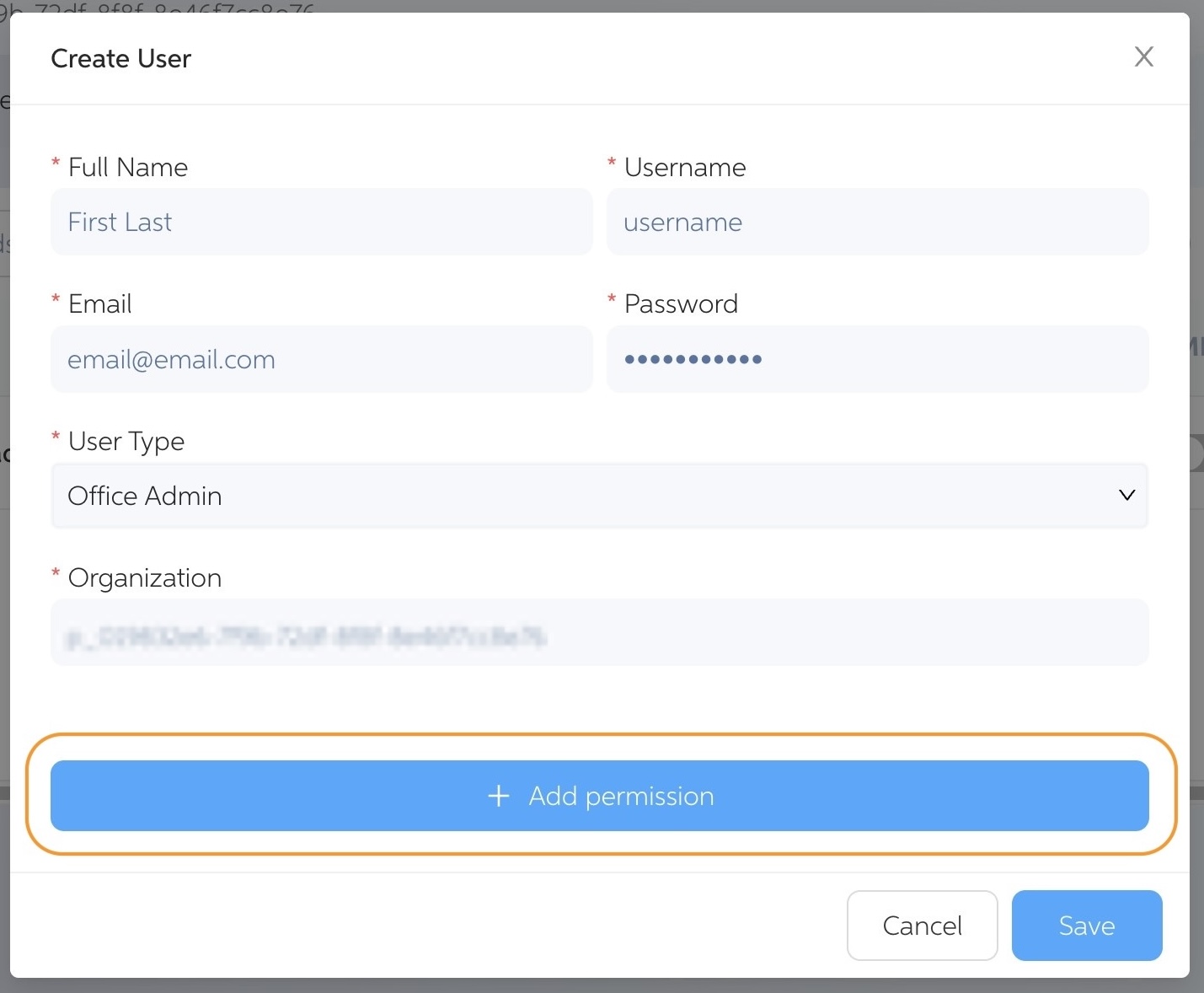
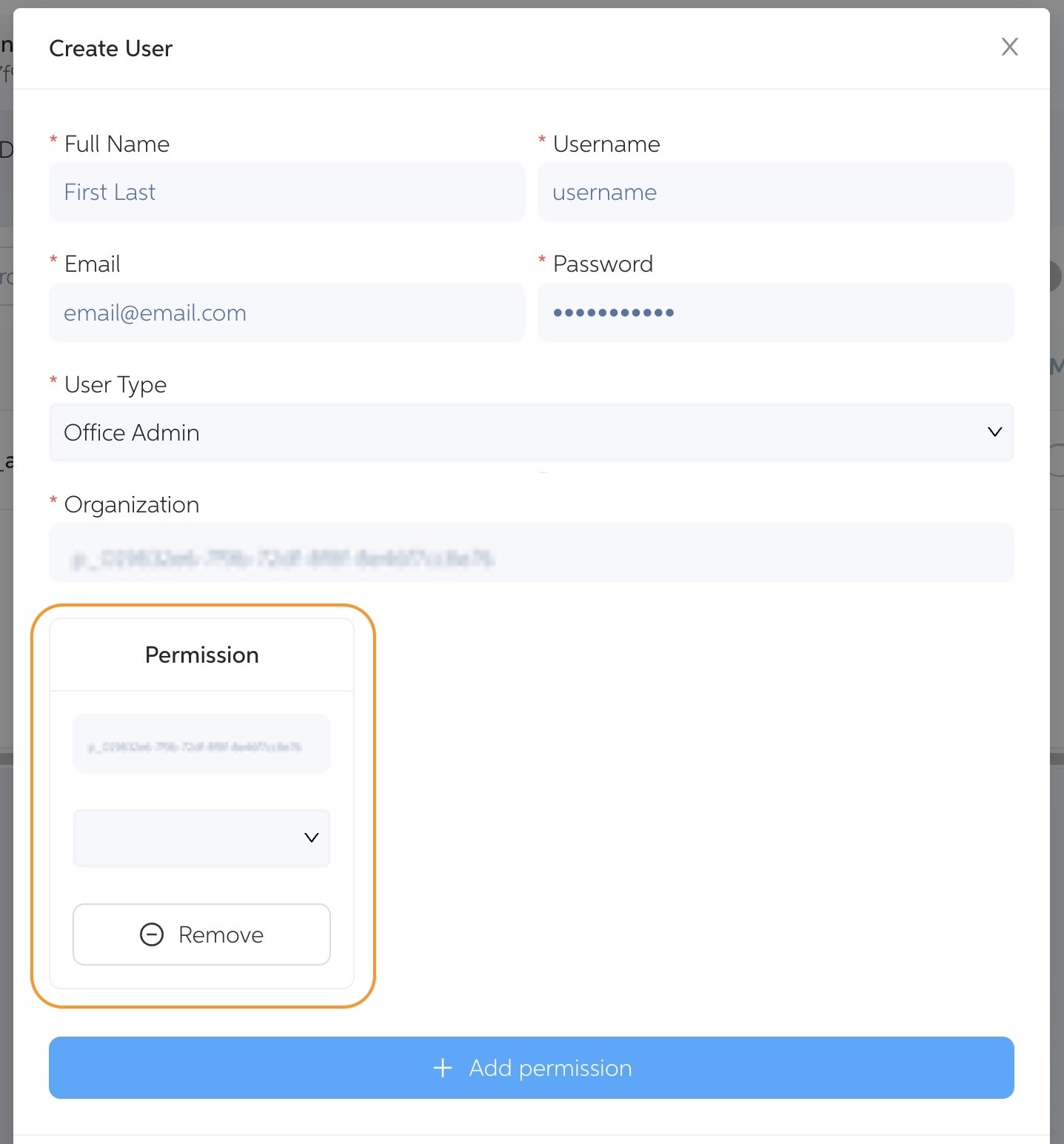
Finalize the setup by clicking the Save button.

Precheck will not determine if a provider is in/out-of-network. Currently those details are accessible via the checkbox to show Out of Network.

The Instant Breakdown feature allows you to manually search a patient’s benefit information. When you have the insurance information, you can generate an instant breakdown by filling in the form fields.
The Instant Breakdown feature allows you to manually search a patient’s benefit information. When you have the insurance information, you can generate an instant breakdown by filling in the form fields.

Patient insurance information is pulled from your PMS and re-updated daily in the morning.
We first run an automated process with hundreds of payers that we have setup using the existing PMS information. The other option is that we support even more payers using the office's login credentials. In the case of both options being available and setup, the office login method will take precedence over the automated process.
No, you may manually do so when needed. However full and condensed reports can be saved into your PMS whenever desired.